Male Infertility
A common misconception is that infertility is primarily a woman's "problem". In fact, male infertility affects the same number of couples as female factor infertility. An additional 25% of couples who seek treatment have more than one factor or condition affecting their ability to reproduce.
If your wife or partner has unsuccessfully attempted to get pregnant with regular, unprotected sex after trying for a year, or if you are concerned about your fertility, then we recommend that you consult a fertility specialist as soon as possible, especially if you have:
- Any problem related to sexual function, erection or ejaculation problems, low sex drive
- If you feel pain in the testicles
- If you notice a lump or your testicle area is swollen
- If you have a history of sexual, testicular or prostate problems
- If you had surgery related to your reproductive system
- If you are over 40 years old
The causes of male infertility are:
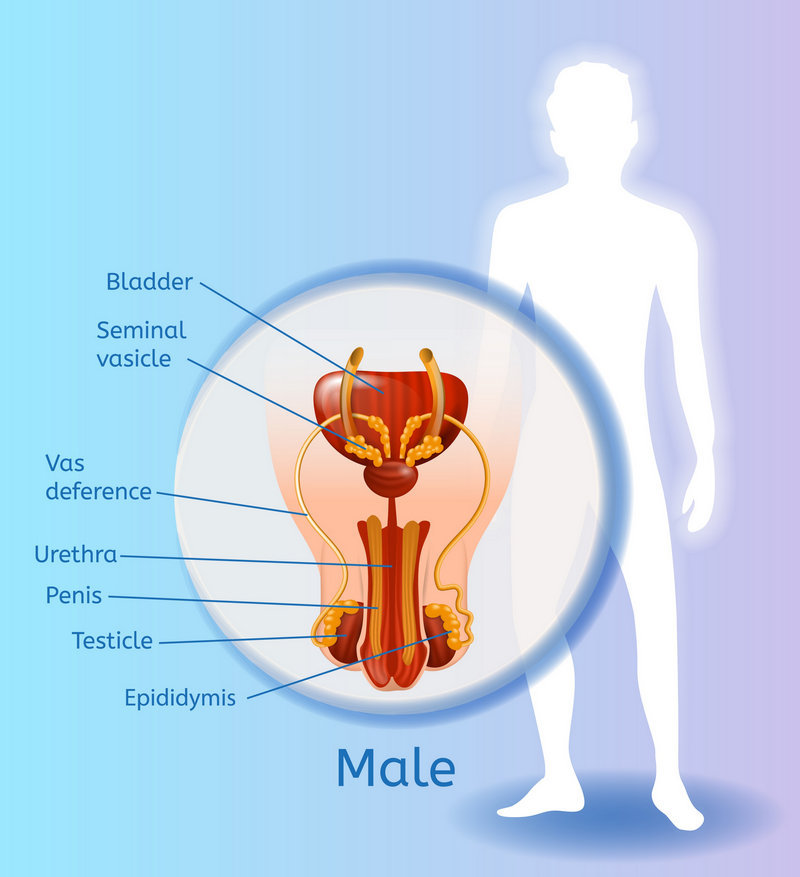
- A problem with testicular production of sperm
- No sperm (azoospermia), a condition where no sperm is found in the semen due to poor testicular function or obstruction of the male reproductive tract. It is the most challenging male infertility condition to manage.
- A blockage or absence of the duct for sperm (vas deferens) from the testicles
- Varicocele, a dilated vein in the scrotum
- A hormonal imbalance
- Lack of sperm mobility or function
- Previous injuries or health factors
- Ejaculation disorders
- Tumors and cancer therapy (chemotherapy, radiation therapy, aggressive surgery)
- Other conditions such as chromosome abnormalities, advanced age, stress, sexually transmitted diseases, being overweight, smoking, illicit drugs, alcoholism, trauma, radiation, and exposure to toxic chemicals
To identify male infertility, we analyze a semen sample for the volume of semen, the concentration of sperm, the percentage of actively moving sperm (motility) and the number of typically shaped sperm (morphology). A DNA fragmentation test will give us valuable information. It is not common, but male hormone testing may be recommended, too.
Even if one or more of these measurements is lower than normal, a man may have normal fertility. A semen analysis alone cannot fully predict a couple's fertility. When male factor infertility is identified, we recommend a complete infertility evaluation of the woman.
Men with Genetic Disorders
Recent molecular genetic studies suggest that unexplained infertility in men may be due to underlying genetic disorders. At our reproductive center, we provide advanced genetic evaluation for infertile men. This evaluation includes a blood test for karyotype analysis to evaluate anomalies in the chromosomes, a Y-chromosome microdeletion analysis, and a CFTR mutation screening to identify cystic fibrosis or related disorders. Our andrologists/urologists and geneticists provide professional counselling to all couples before and after the genetic screening to address concerns about their general and reproductive health and the health of their future children.
Men with Spinal Cord Injury or Ejaculatory Disorders
Men with spinal cord injury or other neurological conditions may have severe impairment to their sexual function, particularly in the ejaculation of semen. We provide special options to retrieve sperm for assisted reproduction, such as ejaculation by vibrostimulation, electro-ejaculation, and percutaneous needle aspiration of sperm on an outpatient basis.
Book a Free Online Consultation with Dr Thanos Paraschos and his team
Male Infertility Clinic at EmBIO IVF

Our Male Infertility Clinic is headed by renowned urologists who specialize in the full range of evaluations and treatments in male reproductive medicine with an emphasis in fertility preservation for cancer patients, treatment of severe male factor infertility, treatment of men with clinical hypogonadism (symptoms of low testosterone), as well as sexual dysfunction.
Our urologists are also specially trained in advanced microsurgery of the male reproductive system.
Our urologists work hand-in-hand with EmBIO IVF using a team approach to determine the best option for individuals and couples. Whether a couple is seeking a vasectomy reversal or the male individual requires treatment for common conditions such as varicocele -- we will carefully guide them through all treatment options available.
Treating Male Infertility
If male factor infertility has been diagnosed through semen analysis, there are several approaches for treatment, including drug therapy, surgical therapy, ART, ICSI and donor sperm.
- Drug Therapy. Hormonal imbalances affecting the development of sperm can usually be successfully treated with drug therapy.
- Surgical Therapy. When a physical barrier prevents sperm production and maturation or ejaculation, a surgical procedure may be the most effective means of retrieving the sperm for insemination. These surgical procedures involve the retrieval of the spermatozoa using a thin needle.
- ART - Assisted Reproductive Technology. The female partner will often undergo intrauterine insemination (IUI) or in vitro fertilization (IVF) to treat certain types of male infertility. In cases where IVF is involved, it is often performed using ICSI.
- ICSI - Intracytoplasmic Sperm Injection. Intracytoplasmic sperm injection (ICSI), is used in cases where sperm are insufficient, do not swim properly, or have an abnormal shape that prevents them from penetrating the egg. An embryologist uses a microscope to carefully select, immobilize and draw a single healthy sperm into a pipette. After stabilizing the mature egg of the female partner, the embryologist carefully injects the sperm into the egg. This process takes less than ten minutes and does not damage either the egg or the sperm.
- Donor Sperm IVF. An alternative approach to male factor infertility is using a donor from one of several national sperm banks. We can provide information to aid your search for a sperm donor. Once a donor is identified and the sperm is available, the female would most likely go through an IVF cycle in combination with ICSI.
- Vasectomy Reversal. A vasectomy can often be reversed through surgery. A vasectomy reversal rejoins the vas deferens. It is performed under light sedation with the aid of a microscope. Pregnancy rates following a vasectomy reversal are generally over 50%.
- Varicocele repair (tangled blood vessels in the scrotum)
- MESA (micro epididymal sperm aspiration)
- PESA (percutaneous epididymal sperm aspiration). A procedure involving a needle inserted into the epididymis in an effort to locate and aspirate a pocket of sperm.
- TESA (testicular sperm aspiration) or testicular biopsy. A needle biopsy of the testicle in which a sample of tissue is taken directly from the testis and used to extract sperm for IVF or ICSI.
- Testicular microdissection, careful surgical intervention in the testicle to locate any areas of potentially active spermatogenesis. This allows minimal extraction of testicular tissue, which minimizes the risk of permanent damage to the testicles.
- Procedures for fertility preservation (sperm freezing)
For some couples, the use of IVF with donor sperm remains the best option for building a family. Obviously, donor sperm is the only option for men whose testicular biopsy reveals complete azoospermia - no trace of sperm in the testicular tissue. The use of donor sperm may also be considered when genetic screening indicates a possibility of passing on hereditary conditions such as cystic fibrosis to male offspring.

An increased understanding of male factor infertility and the recent advances made in assisted sperm retrieval techniques are now giving men who never thought they could have biological offspring the chance to father a child. Successful fertility outcomes at our center result from a combination of technological advances, scientific expertise and consistent andrology laboratory standards.
Book a Free Online Consultation with Dr Thanos Paraschos and his team

