Mini IVF
Mini IVF is designed to select only a few but high quality eggs and thus reduce the risk of overstimulation, the cost of treatment and the number of injections.
A mini IVF cycle is a cycle in which the patient receives a reduced amount of ovarian stimulation drugs and therefore produces fewer eggs than a cycle of conventional stimulation. We aim for 3-5 eggs instead of the 10-15 eggs produced in conventional stimulation.
It is a completely different approach which relieves the patient of much of the complexity and high costs that accompany conventional protocols.
How mini IVF is performed
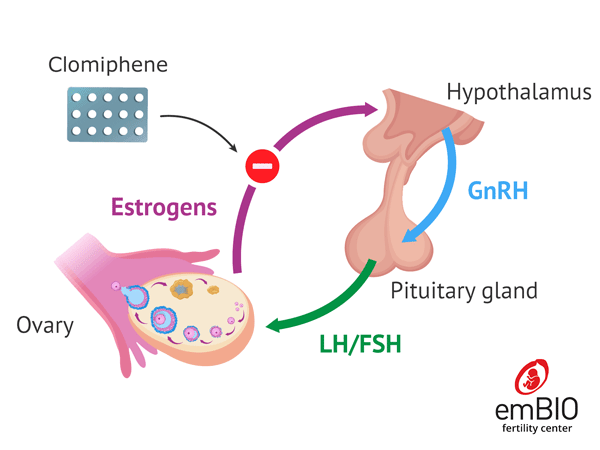
The woman is given oral ovarian stimulation medication along with a small amount of injectable medication. Letrozole or less commonly clomiphene citrate may be used for five days and on the 6th day a low dose (up to 150 units) of injectable gonadotropins may be started until the eggs mature.
Alternatively, we can give exclusively a low dose of injectable gonadotropins from the beginning. The antagonist is normally administered to prevent early ovulation.
The stimulation treatment is normally started on day 2 of the period and the follow-up is exactly the same as a conventional IVF cycle. The cycle is monitored with ultrasound scans and blood tests. When the maturation of the follicles is judged to be satisfactory, an injection of chorionic gonadotropin is given. In 34-36 hours, ovulation is scheduled.
On the same day of the ovulation, sperm collection, processing and fertilization of the eggs will be done either by simple fertilization or microfertilization. The embryos will be monitored by the embryologist until embryo transfer with 3rd day embryos or blastocysts is performed. Due to the small number of eggs collected, it is less likely that there will be leftover embryos to be frozen and used in another embryo transfer attempt.
Advantages of mini IVF
- Prevention of ovarian hyperstimulation syndrome (OHSS)
- Significantly lower treatment costs due to minimal medication requirements
- Reduced physical stress on the body due to lower medication doses
- Targeted egg production - only collecting the number of eggs needed for embryo transfer
Who are suitable candidates for mini IVF?
- Young women under 35 with a tubal infertility factor who have a very good prognosis.
- Women who don't want to take a lot of drugs, but want to increase their chances of having a completely natural IVF cycle.
- Women with polycystic ovaries who want to avoid the risk of overstimulation (although we have other protocols that protect them from this, in which the GnRH agonist replaces the injection of chorionic gonadotropin for final follicle maturation).
- Women who have low ovarian reserve and are unable to produce many eggs with conventional IVF stimulation. Today, this is the main indication for mini IVF.
- Those who would like a lower cost - this is achieved because they will avoid the cost of many drugs
- Those who would prefer not to have to freeze, donate or discard embryos or eggs that will be left over after embryo transfer. They do this because with mini IVF we only produce as many eggs as we need for an embryo transfer.
In general, mini IVF is not recommended for the entire population that needs IVF because it generally has lower success rates than conventional IVF.
There is a study published in the American Journal of Obstetrics and Gynecology in 2016, which revealed that birth rates are 49% in people undergoing mini IVF versus the 63% achieved by patients undergoing conventional IVF.
So we have a 22% lower success rate and this is because the chance of IVF success depends on the number of eggs collected. IVF success reaches its highest rate if 15 to 25 eggs are collected according to a 2017 study in Fertility and Sterility "How many oocytes are optimal to achieve multiple live births with one stimulation cycle? The one-and-done approach".
Although it was previously thought that embryos produced by mini IVF are of better quality, this has not been proven by studies. However, mini IVF does not lose its value in patients with low ovarian reserve in whom even with higher doses we cannot get many eggs, so there is no point in administering them.

